Director of Cardiac Imaging, Bill Shirkey, shares his experience with using handheld ultrasound.

The world is facing a global pandemic with unknown implications, and there’s a new risk factor impacting the heart: COVID-19. Patients with underlying heart disease or diabetes are at higher risk of severe illness for COVID-19.
Because of this, ultrasound of the heart, which can be performed at the bedside, has become a key tool for clinicians while treating and monitoring COVID-19 patients. Ultrasound helps healthcare providers by quickly gathering information on a patient’s heart condition in a consistent, repeatable way. It has proven useful as it is easy to clean and transport in and out of the small, negative pressure rooms being used to isolate patients.
With the cardiac implications of COVID-19 coming to the forefront, GE HealthCare interviewed Bill Shirkey, Director of Cardiac Imaging at Naples Community Hospital System in Florida, to learn more about the use of ultrasound for monitoring patients with cardiac complications and his experience during the pandemic.
Can you just tell us about what your current role is and what it entails?
Bill Shirkey: I’m a unique person here at Naples Community Hospital because I’m an administrative director that does clinical work too. I have administrative director responsibilities, but I do a full day’s worth of scanning on top of it. I basically scan more advanced type of disease or for therapies. I do a lot of 3D and strain work in the outpatient facility. I actually see more oncology and pulmonology patients than I do cardiology patients. Within the hospitals, I’m pretty much the go to person for 3D imaging.
How has COVID-19 impacted the facilities that you oversee?
Bill Shirkey: I have three outpatient offices, 2 office labs (one adult and pediatric). For the outpatient facility, I’ve condensed all testing down to one site and eliminated all non-essential or emergent studies. On the inpatient side, we basically have established a new “echo triage” if you will, to help in determining what type of studies someone needs.
We have also stopped doing studies in the lab. We do all studies portably. We have sequestered our equipment down to one room. And the equipment is all split to what patient it needs to do. Some equipment does [COVID-19] negative people. Some equipment does COVID-19 positive only. And then I have the handheld units that I use basically for point of care echo’s, which is for anybody that gets an echo order that is not negative. So, we consider everyone positive unless they’ve been tested for negative. We go through the orders every morning. The staff does with me. I point the study to certain directions. So, it’d either be point of care handheld study, a point of care study with a very limited Doppler, a limited study, or a full study.
Can you tell us about the “echo triage” process you and your team have developed?
Bill Shirkey: The whole point of it is to limit time in the room. Particularly with patients, we don’t know what their status is. They are pending, called a PUI (person under investigation), or COVID positive patients. The whole point is to limit down our time in the room. That’s why I really put into place the handhelds. Because there’s a certain number of patients that come in that really don’t have any cardiac history or they’ve had previous studies that are normal studies for the most part. Or they are coming in with certain indications: chest pain, palpitations, abnormal EKG, shortness of breath, syncope. Things like that, I feel that those patients are okay to get just a handheld study.
What we do is we do that study, upload it quickly to have a cardiologist take a quick look at it, to make sure that there’s no other further information needed. Because we are in full gear usually while we are doing the handheld studies, it is markedly easier to do, because the gear is quite hot and uncomfortable, and it does affect your ability to concentrate well. My feelings are that having to bring a regular size equipment in, move the room around, get the patient adjusted in the bed, and then having to deal with all the cleaning everything involved with the full blown equipment it is too time extensive and exhausting. And it really doesn’t give you much more clinically than you could give from a handheld in certain situations.
So, should I do a point of care study with a handheld and I come across something like aortic stenosis, I call down to my team while I’m in the gear in the room, and I have them bring up a certain piece of equipment for me to use so I can do the Doppler interrogation. Basically, I finish my study on the point of care, and they hand off the machine to me if I need it, which at this point that’s only happened 10% of the time. Then I do the specific focus Doppler interrogation. I’m not doing a full scan again, it’s just because that system does not have Doppler at this point. Then I just bring that system in, so we don’t have to expend more PPE. That’s just how we do it.
We have someone also, a technologist that works in the office here, they are kind of a mediary between the cardiologist and the technologist if need be. They would let the cardiologist down here know that, “hey, there was a point of care study done by the handheld unit, can you take a look and see if you need any further information?” Like I said, I haven’t had any cardiologist ask for more information.
On 10% of the cases, which has been involving me mostly with those cases, I’ve found two, maybe three patients that have had aortic stenosis, so I had to do an evaluation for aortic stenosis. But, everybody else’s have been clean, and I haven’t had to do any other reimaging. That’s a pretty good for us to have limited times in the room. So, you’re talking with that system I’m in the room 10 minutes max. With the other system, if I had to boot it up, boot it down, clean it all – because we do a clean in the room and a clean out of the room – you’re talking extensive time, like over an hour.
Can you tell me about the first COVID-19 patient that you treated? Just what that experience was kind of like and what you saw and just a little peak into the experience?
Bill Shirkey Yes, absolutely. The first COVID patient we had here, took out about 60 staff members for quarantine because she came in and presented as a myocardial infarction (heart attack) but ended up having COVID-19.
Here we have a lot of negative pressure rooms, so when you go up to units; they’re all sequestered to two units at each hospital right now. You go up there and it’s all closed off and there’s really nobody but the patient in the room. When you get there, you usually are approached by a couple people because you’re going in with PPE and they don’t want to expend PPE unnecessarily so they will probably have you do a few tasks for them also other than just doing your echo.
The other day I did one, I had to get the linens for the linen guy. I had to get the lunch from the nurse. I had to deliver some medication from the nurse. And then when I got in there, I had to take care of the patient because no one really comes in, so the patient needed some things too. So, that all happened even before I started my echo. But fortunately, I had the system all powered up name, ready to go. I did the echo and was out of the room in 10 minutes. That was that and it was great because I didn’t have to do any furniture moving, I didn’t have to lug anything around and like I said the cleaning/sanitizing time on the unit two minutes max. I mean it’s great, and the images were awesome. I would say the image quality honestly is not terribly, terribly far off a regular system if you’re a good sonographer.
What were you looking for, specifically when you put a probe on a cardiac COVID patient, what are you looking for in the heart?
Bill Shirkey: My first thing I’m going to be looking for is left ventricular function because myocarditis is a common issue with COVID-19. Function and size are always going to be the important things off the bat. And then I look at all the valves with color and I’m also looking for any kind of effusions, pericardial effusion.
Are you scanning these patients every day? How many patients are you scanning right now a day?
Bill Shirkey: Yeah, pretty much. Today, I think we did, so far, we’re a little slow right now, I think we did 10 at this point. Unfortunately, with our population here, we are Naples, Florida, so it’s an older population, so you are going to have more acquired heart disease here. I would think other areas of the country, you could probably get away with a lot more than we do, because you won’t have as much acquired heart disease.
I would just like to say that you must create a plan or a protocol and you have to have good cohesion with your medical director. You both have to be kind of on the same page and comfortable with the work you provide. This will never work if there’s not a high level of trust, which that must be whenever you bring anything new into an established lab like this. Even 3D imaging, things like that, there’s got to be a high level of trust and a high level of quality. Therefore, I don’t have everybody doing it. I don’t have everybody doing handhelds and I would not because it would not work. This is for your senior sonographers who understand pathology, understand what the cardiologist needs to look at or is going to want to see, and then it works well.
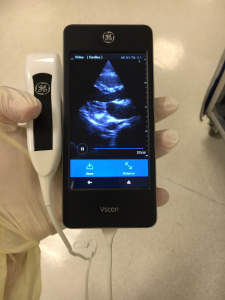
Is there anything else that you want to mention in the role that your Vscan Extend™ has been playing while you’re treating COVID-19 patients?
Bill Shirkey: It provides a good mechanism, particularly for COVID-19 positive patients. I don’t really think on most of these people you need to bring in a full-blown unit and do a full Doppler evaluation on patients that are critical. They just need to know function or effusion. The whole point is to limit the time in the room. We already know that viral load is an important aspect as why people do not do well. Anything to lessen the amount time in the room and exposure to viral load is something a system should take a hard look at doing. really feel this whole process change that we’ve gotten into our department and been working through this scenario now, we’ve been very fortunate, we’ve had time to plan and kind of perfect our techniques and how we work.
Do you think using handheld ultrasound it makes it easier on the patients? Has there been any sort of reaction from them on that front since they can see the scan happening?
Bill Shirkey: I do feel it’s easier on the patient. They may not perceive it, but I think it’s easier because it’s easier on the technologist. Whenever you make it easier on the person performing it, you make it easier on the person receiving it.
Do you think you’ll be applying these learnings beyond COVID-19?
Bill Shirkey: I do foresee, in this area, this will probably be something that stays with us past COVID-19. Well, COVID-19’s going to be here for a while, but in the future, I even see this as how I would probably get a lot of observation patients out of the system or discharged. I could go down to an observation unit in the morning and if they had 5 patients, I’d just do all the observation patients with the point of care. And if they feel they need further imaging that’s imperative, they could schedule them as an outpatient and then discharge the patient. And then I’ve also talked to them a bit about working with the cardiologist on the consult side, on the outpatient end, and if they had any need while they are consulting a patient, we could easily go in with a handheld and do a point of care echo right then and there. It would only take 5 minutes or so. It does open you up a lot more ability to get a look quickly and then determine where you want to go from there.




